Product is injectable, in powder form, needs reconstitution before use.
This PRODUCT IS INTENDED FOR RESEARCH PURPOSES ONLY. It is designed for in vitro testing and laboratory experimentation exclusively. All the information provided on this website is purely for educational purposes. Under the law, any form of bodily introduction of this product into humans or animals is strictly prohibited. It is essential that only licensed and qualified professionals handle this product. This product is not intended to be used as a drug, food, or cosmetic. It must not be misbranded, misused, or mislabeled as such. Its purpose and usage are solely confined to research and scientific investigation.
KPV Peptide Structure
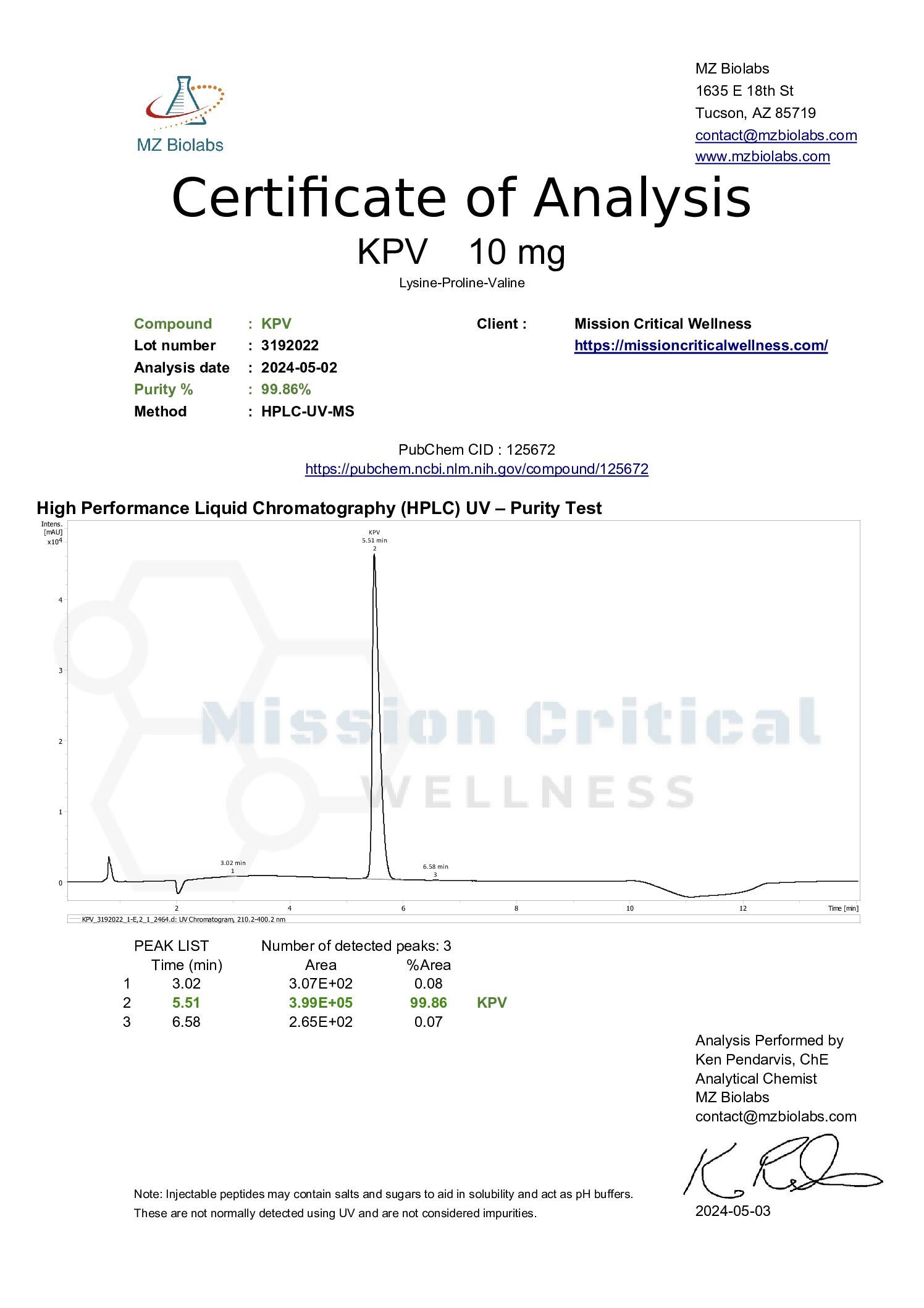
- Amino Acid Sequence: Lys-Pro-Val
- Molecular Formula: C16H30N4O4
- Molecular Weight: 342.43 g/mol
- PubChem CID: 125672
- CAS Number: 67727-97-3
- Synonyms: MSH (11-13), ACTH(11-13), alpha-MSH(11-13)



Reviews
There are no reviews yet.